Physicians experience many emotionally challenging situations in their professional lives that affect their emotional state through emotional contagion and social evaluation processes. Successful emotional regulation is critical to maintaining health, achieving well-being, promoting resilience, and preventing burnout and compassion fatigue. Despite the alarmingly high rate of stress-related illnesses among physicians that affect physical health status and outcomes such as physician performance, quality of care, and patient satisfaction, physicians are more likely to be emotionally affected. There is a lack of research on how people deal with difficult situations. For instance, emotional involvement can interfere with medical objectivity, impair judgment, and lead to a tendency to over-treat patients. Physicians have also been shown to reduce pain while observing visual stimuli representing physically distressing situations. The authors argue that this downregulation is required for painful therapy. Therefore, emotional distancing has long been a desirable emotional state for physicians. Medical students and residents learn to control their emotions through role models and clinical practice. Indeed, several studies have reported a decline in empathy in medical schools and residents; however, there are also conflicting results.
Our DBMR team investigated the chronic fatigue syndrome market and witnessed that North America dominates the chronic fatigue syndrome market because of changing lifestyles and increasing healthcare expenditure rise in the availability of funds for research, huge patient population, increasing healthcare expenditures, well-developed healthcare sector and government support for research & development in this region. Also, Asia-Pacific is the highest-growing region in terms of growth in the market due to the huge patient population, chronic fatigue syndrome market, and the presence of huge opportunities in this region.
To know more about the study, kindly visit: https://www.databridgemarketresearch.com/reports/global-chronic-fatigue-syndrome-market
Emotional engagement, especially empathy, is critical for patients and clinical outcomes as it is associated with clinical competence and performance and the quality of the doctor-patient relationship:
Patients with empathetic physicians reported more disease-specific information and concerns and improved diagnostic accuracy. Physician empathy has also increased patient participation, adherence, and satisfaction with treatment, making treatment more effective. In addition, empathy is associated with increased patient empowerment, improved communication skills, better decision-making, better disease management, better health, reduced anxiety, and improved patient quality of life. In fact, two randomized controlled trials have shown that physician empathy boosts a patient's immune response and reduces the duration and severity of colds. Patients and healthcare systems, as well as physicians themselves, can benefit from medical empathy. Empathy is linked to health, compassion, happiness, and quality of life, but causality is still unclear.
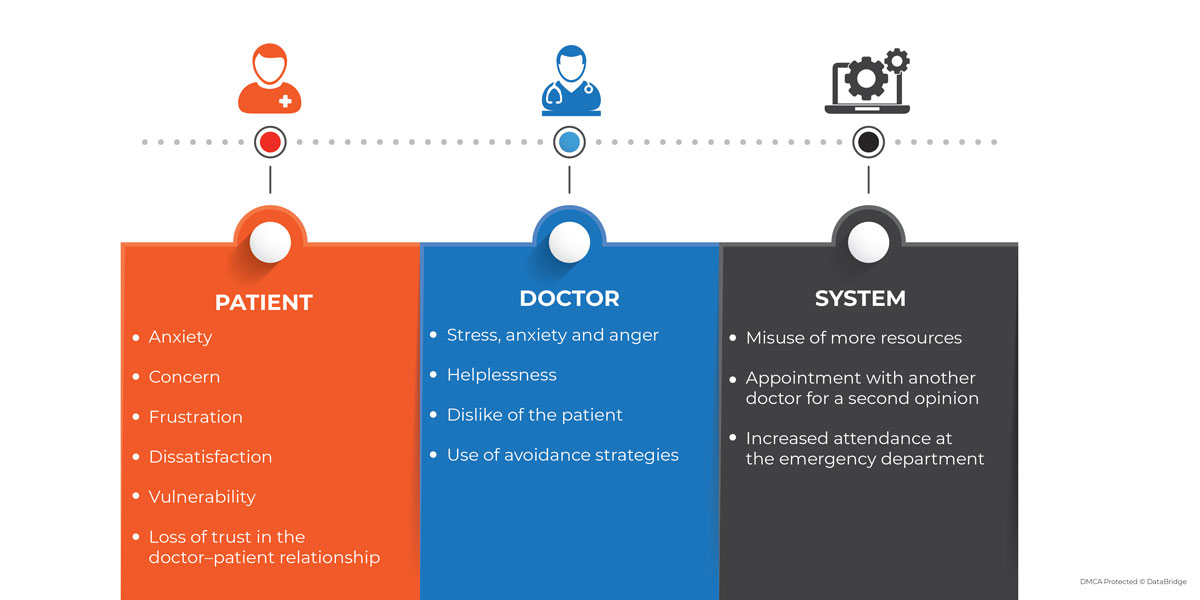
Many studies have shown that emotionally challenging situations, in combination with different coping strategies, can have severely deleterious effects on physicians, patients, and the healthcare system. Stress-related disorders such as burnout, depression, substance abuse, and suicide are significantly more prevalent in physicians in these patients compared to the general population. Emotionally charged social interactions are thought to be one of the primary reasons for the extremely high occurrence of these disorders. In turn, the physician also leaves negative consequences for numerous clinical outcomes such as quality of care, physician performance, patient satisfaction, and treatment adherence.
Our DBMR team investigated the substance abuse and addiction treatment market and witnessed that growing special designation from regulatory authorities is a major factor fostering the market growth. Additionally, it has been witnessed that North America dominates the market due to the earliest adoption of innovative healthcare technologies, increasing research and development, high prevalence rate, growing adoption of novel dosage forms, and increase in healthcare awareness among people.
To know more about the study, kindly visit: https://www.databridgemarketresearch.com/reports/global-substance-abuse-and-addiction-treatment-market
Refusal is a basic human right, as is asking for treatment the physician may consider futile; physicians can resolve the problem a big percentage of the time.
Eduardo Bruera, MD, Chair, and Professor in MD Anderson's Department of Palliative Care and Rehabilitation Medicine said, "Patients have to make decisions under extremely difficult circumstances, particularly when they are getting to the level of having very advanced cancer. The emotional component drives a lot of the decision-making. Cognitive aspects-where my cancer is and my odds-are only part of patients' decision-making, so we need to understand their emotions."
There is always an emotional impact on the oncologist and the palliative care team as well, who may feel disappointed by the fact that patients are not welcoming or accepting their recommendations and knowledge whole-heartedly. There is a process of understanding that need to be addressed properly:
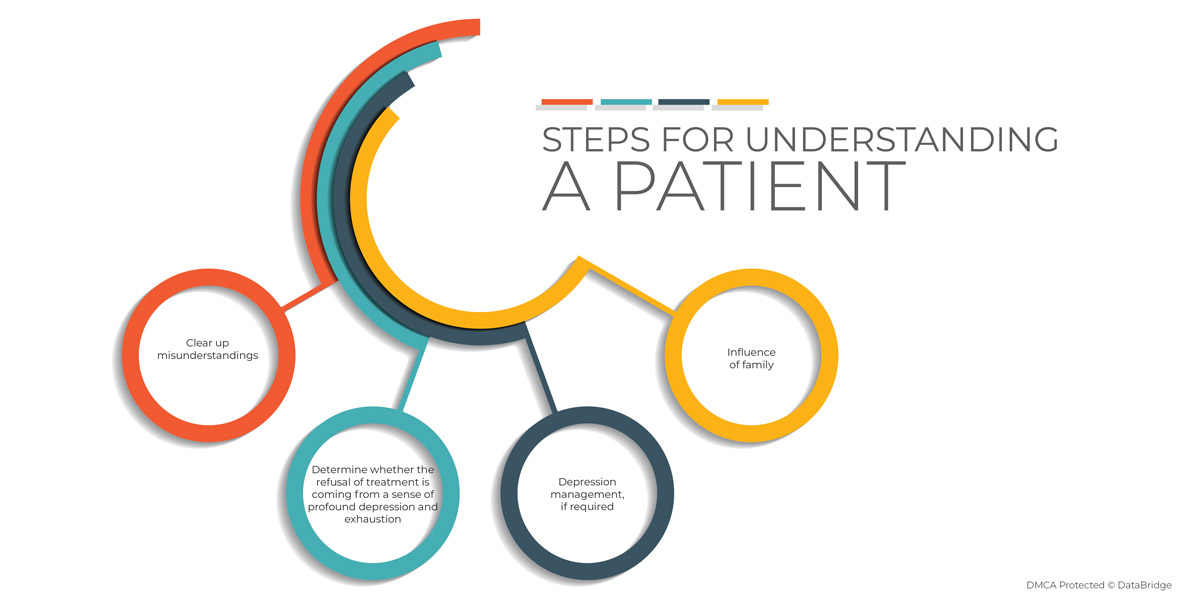
Decision-making does not follow precise pathways or clinical guidelines, he continued. "Clinical care guidelines are useless in situations that call for personalized care. What we are managing is the person, and many factors are involved with the decision that has nothing to do with the disease or the stage. What's important for the oncologist to understand is that decision-making is always personal, and we don't understand all the personal aspects that impact that."
Sometimes it gets difficult to understand a challenging interaction. Numerous different problematic interactions occur on a daily basis. These challenging interactions may arise because of discrepancies in expectation, perception, or communication between the patient and medical practitioner and could be caused by the doctor, the patient, or both.
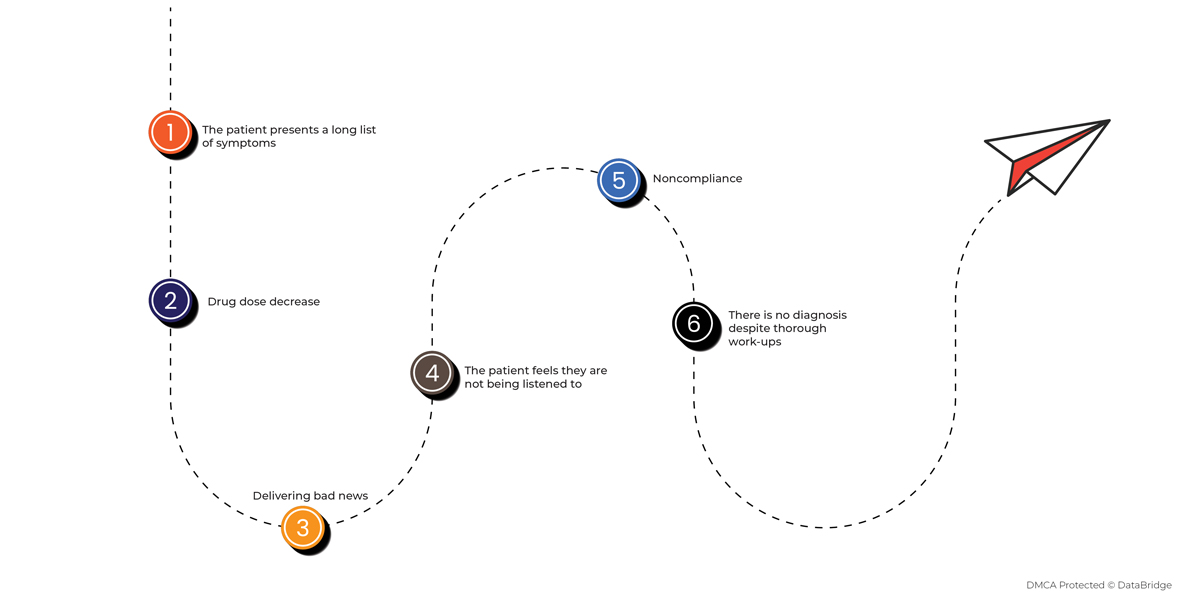
In reality, a challenging interaction between patients and doctors should be considered within the healthcare system in which it occurs. Patients search for professional help as they are in pain or are concerned. It is expected that when the patient, the doctor, and the system interact, a complicated situation can arise.
There are various tips that can be managed or executed to manage these kinds of situations in a better way:
- Paying attention to non-verbal communication
- Discuss with colleagues and do not hesitate to seek additional training should this be required
- Looking for signs of anger or distress
- Create bridges of communication and trust
- Explain the difficulty and try to find common ground
- Ensuring safety and maintaining control
- Help your patient get emotional control
- Giving importance to solutions and resolving areas of disagreement
Case Study:
Patient Background- Mr. and Mrs. Brown, whose infant son, Sam, was diagnosed with Tay-Sachs, a fatal genetic degenerative neurological condition, were primarily involved in decision-making about almost every aspect of their son's care.
Treatment Process For the Patient- Admitted for three months, followed by transplantation. Their parents were in a dilemma about whether to put him into mechanical ventilation
The doctor tried to comfort the parents and make them comfortable while they are on such a vulnerable point. Meanwhile, they are having a conversation:
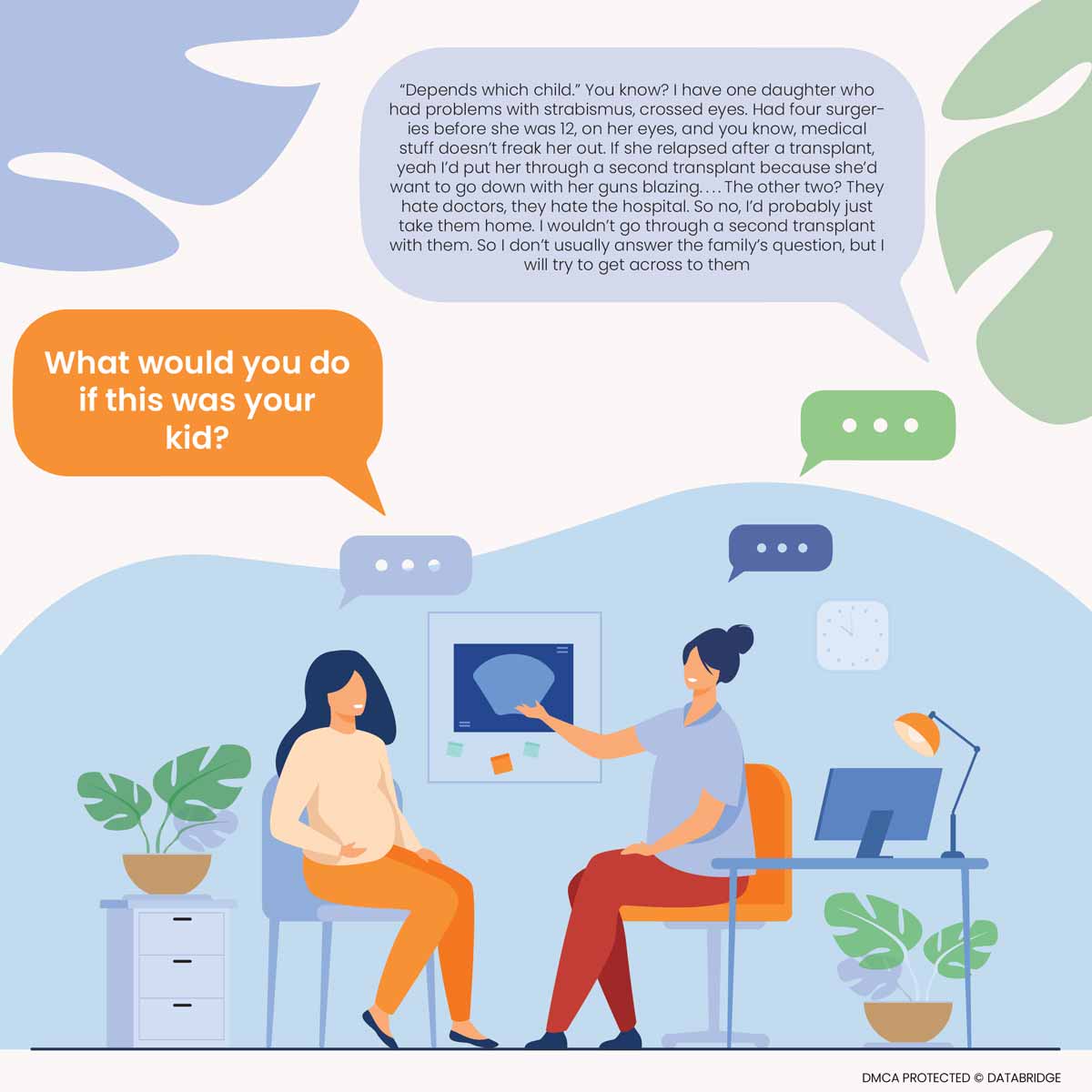
Thus, like these, several cases demand doctors' sympathy, and it is essential to understand patients' situations so that they can believe in themselves and accelerate their confidence. Every patient who refuses treatment has some underlying causes that need to be addressed by the physician. Recovery is essential, and understanding their situation will help them quickly. Future studies should target a broader range of physician-patient interactions, using momentary assessments to prevent recall bias and enable the detection of more implicit emotions and emotion regulation. Future studies should observe the effectiveness of emotion regulation strategies, additional emotion regulation abilities such as flexibility and repertoire variability, and the influence of the presence of other people and related situational variables.









