Global Ai Based Medical Billing Fraud Detection Market
Market Size in USD Billion
CAGR :
% 
 USD
1.19 Billion
USD
5.53 Billion
2024
2032
USD
1.19 Billion
USD
5.53 Billion
2024
2032
| 2025 –2032 | |
| USD 1.19 Billion | |
| USD 5.53 Billion | |
|
|
|
|
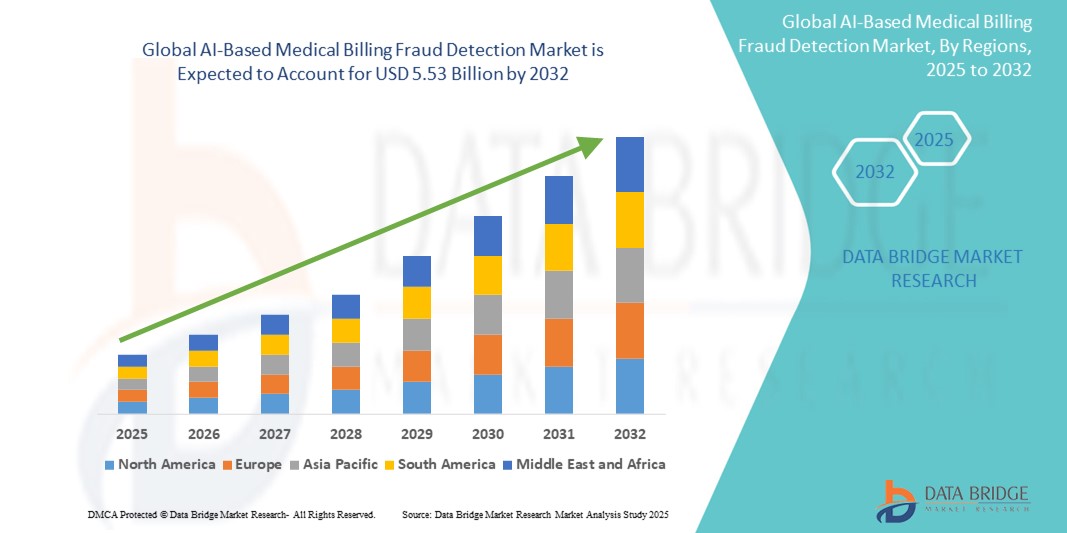
AI-Based Medical Billing Fraud Detection Market Size
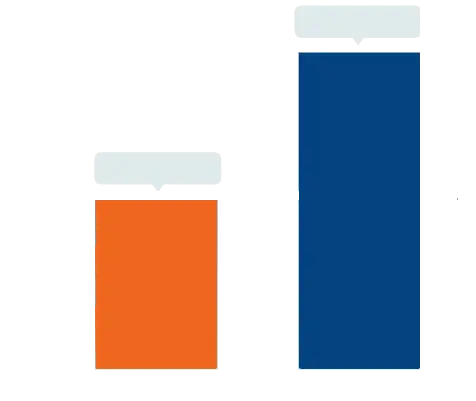
- The global AI-based medical billing fraud detection market size was valued at USD 1.19 billion in 2024 and is expected to reach USD 5.53 billion by 2032, at a CAGR of 21.20% during the forecast period
- This growth is driven by factors such as the increasing incidence of healthcare fraud, rising healthcare expenditures, and growing adoption of AI and analytics technologies to enhance billing accuracy and reduce financial losses
AI-Based Medical Billing Fraud Detection Market Analysis
- AI-based medical billing fraud detection systems leverage machine learning and data analytics to identify anomalies and prevent fraudulent claims in healthcare billing, ensuring compliance and financial integrity
- The market growth is significantly driven by increasing healthcare fraud cases, rising healthcare costs, and the growing need for automation and accuracy in medical billing processes
- North America is expected to dominate the AI-based medical billing fraud detection market with a market share of 45.5%, due to advanced healthcare IT infrastructure, high adoption of AI technologies, and a strong presence of key market players
- Asia-Pacific is expected to be the fastest growing region in the AI-based medical billing fraud detection market with a market share of 16.5%, during the forecast period due to the rapid expansion of healthcare infrastructure, increasing digitalization, and rising fraud awareness
- Software segment is expected to dominate the market with a market share of 60.5% due to its ability to automate complex billing processes, enhance detection accuracy, and reduce manual errors
Report Scope and AI-Based Medical Billing Fraud Detection Market Segmentation
|
Attributes |
AI-Based Medical Billing Fraud Detection Key Market Insights |
|
Segments Covered |
|
|
Countries Covered |
North America
Europe
Asia-Pacific
Middle East and Africa
South America
|
|
Key Market Players |
|
|
Market Opportunities |
|
|
Value Added Data Infosets |
In addition to the insights on market scenarios such as market value, growth rate, segmentation, geographical coverage, and major players, the market reports curated by the Data Bridge Market Research also include import export analysis, production capacity overview, production consumption analysis, price trend analysis, climate change scenario, supply chain analysis, value chain analysis, raw material/consumables overview, vendor selection criteria, PESTLE Analysis, Porter Analysis, and regulatory framework. |
AI-Based Medical Billing Fraud Detection Market Trends
“Advancements in AI Algorithms & Predictive Analytics for Fraud Prevention”
- One prominent trend in the evolution of AI-based medical billing fraud detection is the increasing integration of advanced machine learning algorithms and predictive analytics
- These innovations enhance fraud detection by enabling systems to automatically analyze vast amounts of billing data, identify patterns, and predict fraudulent activities before they occur
- For instance, AI models are now capable of flagging inconsistencies, overbilling, or suspicious patterns in real-time, helping insurers and healthcare providers mitigate financial losses. This is particularly beneficial for detecting complex fraud schemes, such as phantom billing and unbundling
- These advancements are transforming fraud detection processes, improving financial accuracy, and driving the demand for next-generation fraud detection solutions with cutting-edge AI capabilities
AI-Based Medical Billing Fraud Detection Market Dynamics
Driver
“Rising Incidence of Healthcare Fraud and Billing Errors”
- The increasing incidence of healthcare fraud, billing errors, and fraudulent claims is significantly driving the demand for AI-based medical billing fraud detection systems
- As healthcare systems become more digitized, fraudulent activities such as phantom billing, upcoding, and unbundling are becoming more sophisticated, leading to higher financial losses
- The demand for AI-driven solutions is rising as these systems can efficiently analyze large volumes of billing data to detect anomalies and prevent fraud in real-time, ensuring compliance and reducing manual intervention
For instance,
- According to a report by the National Health Care Anti-Fraud Association (NHCAA), healthcare fraud costs the U.S. alone approximately USD 68 billion annually. The growing need for efficient fraud prevention and risk mitigation solutions is driving the market for AI-based fraud detection technologies
- As a result, the rising incidence of fraud and billing errors is fueling the adoption of AI-based solutions, which improve the accuracy and efficiency of detecting fraudulent claims in healthcare billing
Opportunity
“Leveraging AI for Enhanced Fraud Detection and Automation”
- AI-powered fraud detection systems can significantly enhance the accuracy of billing audits, automate the detection of fraudulent activities, and improve overall operational efficiency, enabling healthcare providers and insurers to make better-informed decisions
- AI algorithms can analyze large volumes of billing data in real-time, flagging suspicious claims and identifying patterns of fraudulent behavior, such as duplicate claims, unbundling, or phantom billing
- In addition, AI-powered systems can assist in predictive analytics, helping organizations proactively identify potential fraud risks before they occur, reducing financial losses and improving compliance
For instance,
- In 2025, according to a report from Healthcare Insurance News, AI algorithms are being used to automate fraud detection processes, saving insurers millions of dollars annually by identifying fraud schemes such as overbilling and upcoding. AI’s ability to analyze large datasets quickly allows for more efficient fraud prevention, improving response times and ensuring timely interventions
- The integration of AI in medical billing fraud detection systems can lead to reduced administrative costs, faster claim processing, and increased accuracy in identifying fraudulent claims, ultimately improving the financial integrity of healthcare organizations
Restraint/Challenge
“High Implementation and Maintenance Costs”
- The high cost of implementing and maintaining AI-based fraud detection systems presents a significant challenge, particularly for smaller healthcare organizations or insurance companies with limited budgets
- These AI-powered solutions require substantial investment in software, hardware infrastructure, and ongoing maintenance, which can range from thousands to millions of dollars, depending on the scale of implementation
- This financial barrier may deter smaller healthcare providers and insurers from adopting AI solutions, leading them to rely on traditional methods of fraud detection, which may be less efficient and more prone to errors
For instance,
- In December 2024, according to a report by Forrester Research, the upfront costs of deploying AI-based fraud detection systems can be a significant hurdle for smaller organizations. These costs can include not only purchasing the software and hardware but also training personnel to use these complex systems effectively
- Consequently, the high initial investment and maintenance costs may limit the widespread adoption of AI-powered solutions, especially in regions with less financial flexibility, hindering the overall growth of the AI-based medical billing fraud detection market
AI-Based Medical Billing Fraud Detection Market Scope
The market is segmented on the basis of component, deployment mode, type of analytics, application, and end user
|
Segmentation |
Sub-Segmentation |
|
By Component |
|
|
By Deployment Mode |
|
|
By Type of Analytics |
|
|
By Application |
|
|
By End User |
|
In 2025, the software is projected to dominate the market with a largest share in component segment
The software segment is expected to dominate the AI-based medical billing fraud detection market with the largest share of 60.5% in 2025 due to its ability to automate complex billing processes, enhance detection accuracy, and reduce manual errors. AI-powered software enables real-time analysis of large datasets, helping healthcare providers and insurers identify fraudulent claims more efficiently. In addition, the integration of machine learning and predictive analytics further strengthens fraud prevention capabilities
The descriptive analytics is expected to account for the largest share during the forecast period in type of analytics market
In 2025, the descriptive analytics segment is expected to dominate the market with the largest market share of 41.8% due to its foundational role in fraud detection. It enables organizations to analyze historical billing data to uncover patterns, trends, and anomalies associated with fraudulent activities. This insight is critical for building predictive models and informing strategic decision-making, making it widely adopted across healthcare and insurance sectors
AI-Based Medical Billing Fraud Detection Market Regional Analysis
“North America Holds the Largest Share in the AI-Based Medical Billing Fraud Detection Market”
- North America dominates the AI-based medical billing fraud detection market with a market share of estimated 45.5%, driven, by advanced healthcare IT infrastructure, high adoption of AI technologies, and a strong presence of key market players
- U.S. holds a market share of 42.7%, due to the increasing need for fraud prevention amid rising healthcare fraud cases, high healthcare spending, and government support for adopting AI in healthcare systems
- The availability of well-established regulatory frameworks, such as HIPAA, and growing investments in healthcare technology further strengthen the market, leading to higher demand for AI-based fraud detection solutions
- In addition, the increasing adoption of digital health records and claim automation, along with heightened awareness of fraud risks, is fueling market growth across the region
“Asia-Pacific is Projected to Register the Highest CAGR in the AI-Based Medical Billing Fraud Detection Market”
- Asia-Pacific is expected to witness the highest growth rate in the AI-based medical billing fraud detection market with a market share of 16.5%, driven by to the rapid expansion of healthcare infrastructure, increasing digitalization, and rising fraud awareness
- Countries such as China, India, and Japan are emerging as key markets, driven by their large populations, expanding healthcare sectors, and the growing incidence of healthcare fraud
- Japan, with its advanced healthcare IT infrastructure and focus on cutting-edge technology, remains a crucial market for AI-based fraud detection solutions. The country continues to lead in the adoption of AI and automation in healthcare
- India is projected to register the highest CAGR, driven by rapid healthcare sector growth, increasing healthcare fraud cases, and expanding digital health initiatives aimed at improving billing accuracy and fraud prevention
AI-Based Medical Billing Fraud Detection Market Share
The market competitive landscape provides details by competitor. Details included are company overview, company financials, revenue generated, market potential, investment in research and development, new market initiatives, global presence, production sites and facilities, production capacities, company strengths and weaknesses, product launch, product width and breadth, application dominance. The above data points provided are only related to the companies' focus related to market.
The Major Market Leaders Operating in the Market Are:
- Optum, Inc. (U.S.)
- Cognizant (U.S.)
- Oracle (U.S.)
- Deloitte (U.S.)
- MedAI Solution (U.S.)
- IBM (U.S.)
- SAS Institute Inc. (U.S.)
- MCKESSON CORPORATION (U.S.)
- HCL Technologies Limited (India)
- Infosys (India)
- Wipro (India)
- Tata Consultancy Services Limited (India)
- Accenture (Ireland)
- Capgemini (France)
- NTT Data Group Corporation (Japan)
- DXC Technology Company (U.S.)
- Epic Systems Corporation (U.S.)
- Veradigm LLC (U.S.)
Latest Developments in Global AI-Based Medical Billing Fraud Detection Market
- In May 2025, Optum introduced Optum Integrity One, an AI-driven integrated revenue cycle platform designed to enhance clinical documentation and coding accuracy. The platform automates tasks from point of care through final coding, streamlining the billing process and reducing administrative burdens for healthcare providers
- In April 2025, Oracle introduced advanced AI-driven tools to bolster fraud detection in medical claims. These tools leverage machine learning and natural language processing to analyze vast amounts of healthcare data, identifying patterns indicative of fraudulent activities such as upcoding and phantom billing. By automating the detection process, Oracle aims to reduce false claims and enhance the accuracy of reimbursements
- In April 2025, MedAI Solution highlighted the use of AI in real-time medical billing fraud detection. By employing natural language processing, machine learning, and automation within healthcare revenue cycle management systems, AI can proactively identify and prevent fraudulent billing activities before claims are processed, thereby safeguarding healthcare finances
- In April 2025, Deloitte published insights into the application of AI-powered multimodal technologies in detecting fraudulent behaviors across the insurance claim lifecycle. These technologies analyze various data sources to identify anomalies and potential fraud, helping insurers mitigate financial losses and improve operational efficiency
- In April 2024, Cognizant partnered with FICO to launch a cloud-based real-time payment fraud prevention solution. This AI-powered system aims to help banks and payment providers detect and prevent fraudulent transactions in real-time, enhancing security in the digital payment landscape
SKU-
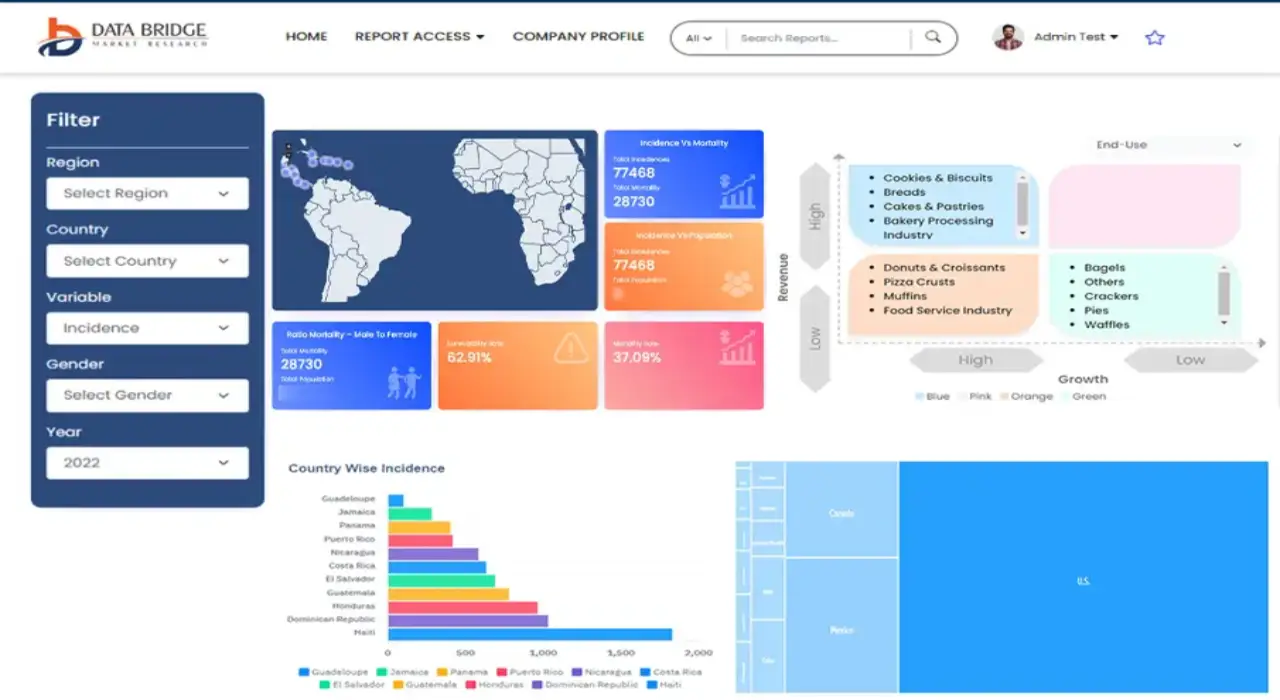
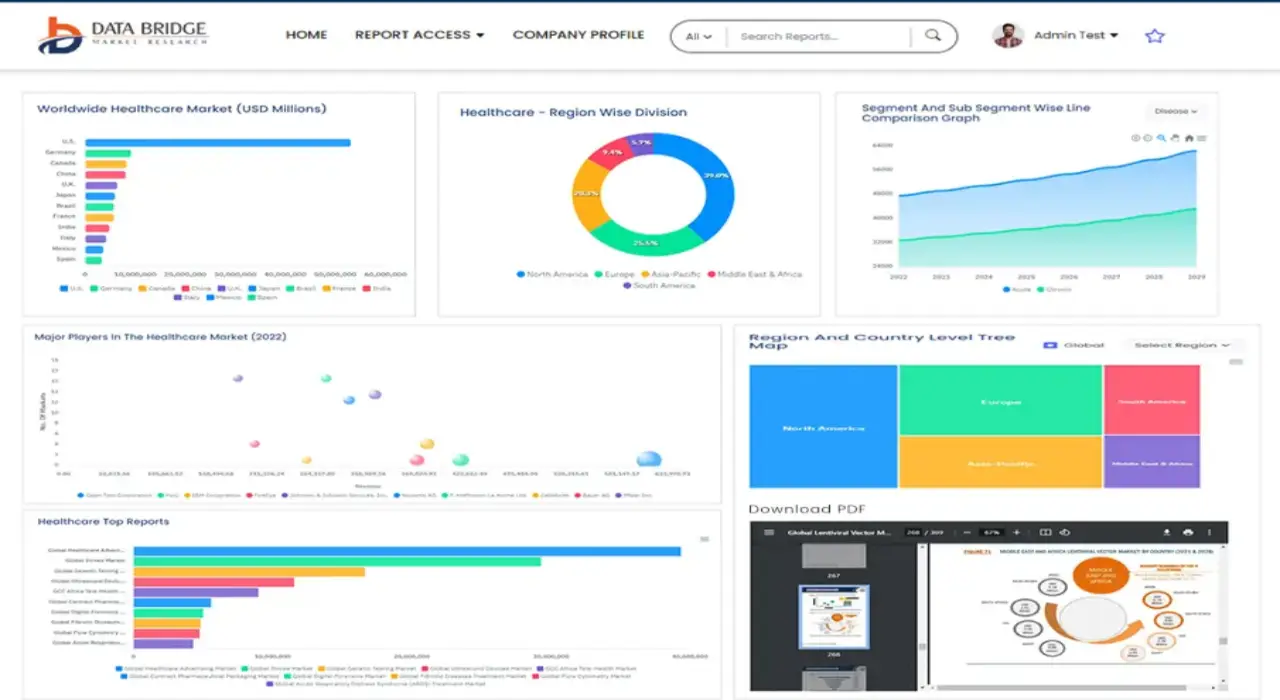
Get online access to the report on the World's First Market Intelligence Cloud
- Interactive Data Analysis Dashboard
- Company Analysis Dashboard for high growth potential opportunities
- Research Analyst Access for customization & queries
- Competitor Analysis with Interactive dashboard
- Latest News, Updates & Trend analysis
- Harness the Power of Benchmark Analysis for Comprehensive Competitor Tracking
Research Methodology
Data collection and base year analysis are done using data collection modules with large sample sizes. The stage includes obtaining market information or related data through various sources and strategies. It includes examining and planning all the data acquired from the past in advance. It likewise envelops the examination of information inconsistencies seen across different information sources. The market data is analysed and estimated using market statistical and coherent models. Also, market share analysis and key trend analysis are the major success factors in the market report. To know more, please request an analyst call or drop down your inquiry.
The key research methodology used by DBMR research team is data triangulation which involves data mining, analysis of the impact of data variables on the market and primary (industry expert) validation. Data models include Vendor Positioning Grid, Market Time Line Analysis, Market Overview and Guide, Company Positioning Grid, Patent Analysis, Pricing Analysis, Company Market Share Analysis, Standards of Measurement, Global versus Regional and Vendor Share Analysis. To know more about the research methodology, drop in an inquiry to speak to our industry experts.
Customization Available
Data Bridge Market Research is a leader in advanced formative research. We take pride in servicing our existing and new customers with data and analysis that match and suits their goal. The report can be customized to include price trend analysis of target brands understanding the market for additional countries (ask for the list of countries), clinical trial results data, literature review, refurbished market and product base analysis. Market analysis of target competitors can be analyzed from technology-based analysis to market portfolio strategies. We can add as many competitors that you require data about in the format and data style you are looking for. Our team of analysts can also provide you data in crude raw excel files pivot tables (Fact book) or can assist you in creating presentations from the data sets available in the report.