Global Healthcare Claims Management Market
Market Size in USD Billion
CAGR :
% 
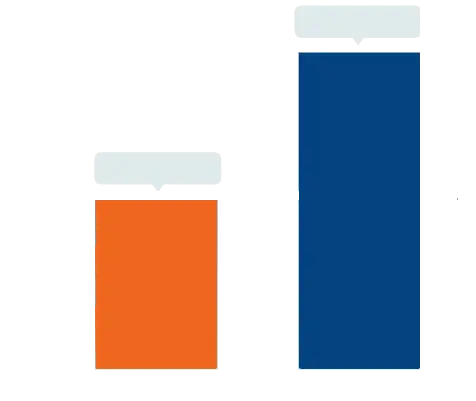 USD
12.29 Billion
USD
18.15 Billion
2022
2030
USD
12.29 Billion
USD
18.15 Billion
2022
2030
| 2023 –2030 | |
| USD 12.29 Billion | |
| USD 18.15 Billion | |
|
|
|
|

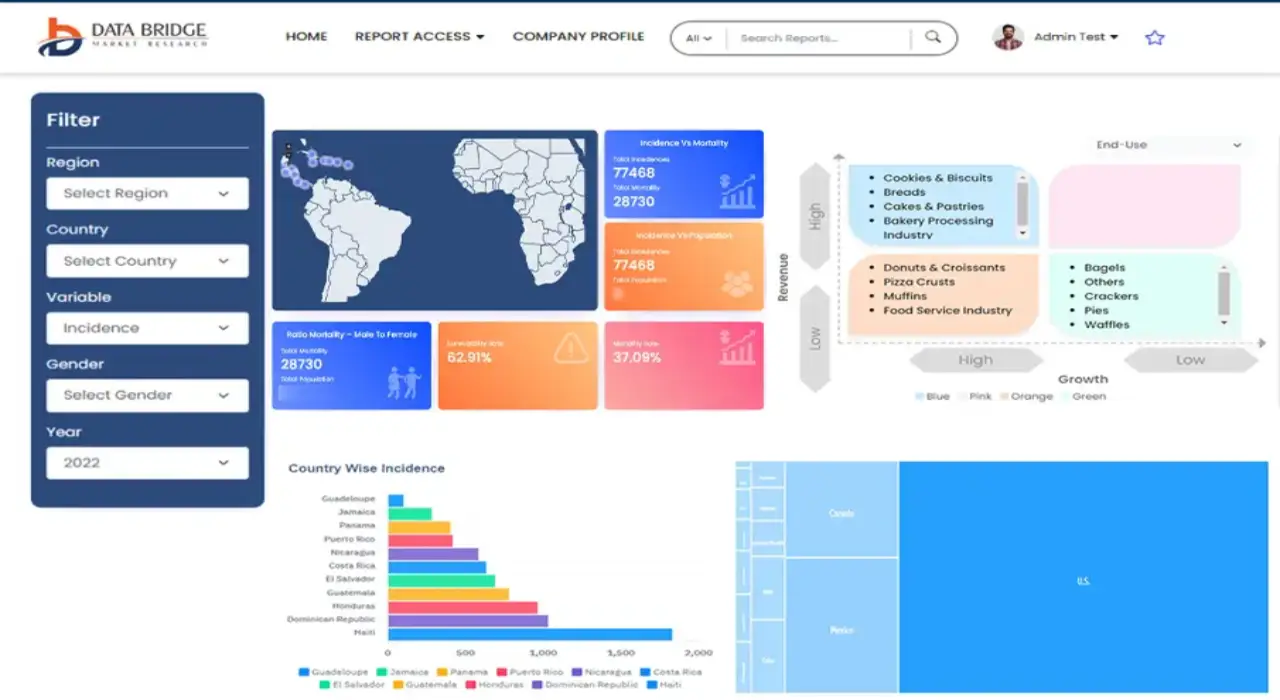
Healthcare Claims Management Market Analysis and Size
Population aging is a major reason for this in many countries, an increasing proportion of the population is over the age of 65, and the prevalence of chronic diseases rises as people age. Furthermore, the economics of health insurance has shifted. The average per capita cost of healthcare in many countries increased at a compound annual growth rate of more than 4%. Insurance plans were initially designed to cover the cost of care for patients with severe, acute illnesses or traumatic injuries, but they now more frequently cover the predictable risks (and costs) associated with chronic illness. Furthermore, advances in healthcare quality (for instance, innovative treatments like gene therapy) frequently result in better outcomes but often raise healthcare costs.
Data Bridge Market Research analyses that the healthcare claims management market, which was USD 12.29 billion in 2022, is expected to reach USD 18.15 billion by 2030, at a CAGR of 5.0% during the forecast period 2023 to 2030. In addition to the insights on market scenarios such as market value, growth rate, segmentation, geographical coverage, and major players, the market reports curated by the Data Bridge Market Research also include depth expert analysis, patient epidemiology, pipeline analysis, pricing analysis, and regulatory framework.
Healthcare Claims Management Market Scope and Segmentation
|
Report Metric |
Details |
|
Forecast Period |
2023 to 2030 |
|
Base Year |
2022 |
|
Historic Years |
2021 (Customizable to 2015 - 2020) |
|
Quantitative Units |
Revenue in USD Billion, Volumes in Units, Pricing in USD |
|
Segments Covered |
Type (Integrated Solutions, Standalone Solutions) Component (Services, Software), Delivery Mode (On-Premise Delivery Mode, Cloud-Based Delivery Mode), End User (Healthcare Payers, Healthcare Providers, Others) |
|
Countries Covered |
U.S., Canada and Mexico in North America, Germany, France, U.K., Netherlands, Switzerland, Belgium, Russia, Italy, Spain, Turkey, Rest of Europe in Europe, China, Japan, India, South Korea, Singapore, Malaysia, Australia, Thailand, Indonesia, Philippines, Rest of Asia-Pacific (APAC) in the Asia-Pacific (APAC), Saudi Arabia, U.A.E, South Africa, Egypt, Israel, Rest of Middle East and Africa (MEA) as a part of Middle East and Africa (MEA), Brazil, Argentina and Rest of South America as part of South America |
|
Market Players Covered |
Athenahealth (U.S.), Plexis Healthcare Systems Inc. (U.S.), Cognizant (U.S.), Oracle (U.S.), Allscripts Healthcare LLC (U.S.), nThrive Revenue Systems, LLC (U.S.), eClinicalWorks (U.S.), Context Healthcare Inc. (U.S.), Optum, Inc. (U.S.), Mckesson Corporation (U.S.), DST Systems (U.S.), Ram Technologies Inc. (U.S.), General Electric (U.S.), Health Solutions Plus (HSP) (U.S.), Conifer Health Solutions, LLC (U.S.), Quest Diagnostics Incorporated (U.S.), Gebbs Healthcare Solutions (India) and The SSI Group, LLC (U.S.) |
|
Market Opportunities |
|
Market Definition
Healthcare claims management is a process that includes tasks like organizing, billing, filling, updating, and processing medical claims related to patients' diagnoses, treatment, and medication. In other words, it is software that manages medical claims and reimbursement processes that is increasingly allowing healthcare providers to maximize their revenues through proper claim management. It is a two-way street between patients, healthcare providers, billing companies, and insurance providers.
Global Healthcare Claims Management Market Dynamics
Drivers
- Growing concerns about data privacy
Despite the market's expected growth, there are growing concerns about data privacy. As technology advances, modern technologies such as cloud, mobile, and next-generation databases are increasingly used to manage, store, and retrieve such claims data. These factors have combined to make healthcare data security a persistent concern for the entire healthcare industry. Rules and regulations governing healthcare data are constantly evolving to ensure patients have the data protection they require and deserve. These are certain factors that boost the growth of the market.
- Digitization of software
Healthcare providers and medical offices adopted digitization at a rapid rate. A lot of information about the patients who receive services each day is being gathered. An adequate system is required for health services to organize, manage, and carry out plans efficiently. The ‘Administrative Errors: Technical Series on Safer Primary Care 2016’ report published by the World Health Organization (WHO) estimated that about 5–50% of medical errors in primary care are administrative errors, further prompting the need for digitization. As a result, there is a growing need for medical billing software.
Opportunities
- Rising duplicate insurance claims
The use of software facilitates communication across various domains and subdomains of hospitals. The programme uses cutting-edge approaches to ensure seamless interoperability between insurance companies and hospitals while managing patient data and information about their treatment. The identical claims and a lack of transparency, the insurance firms reportedly reject about one out of every five claims. Thus, the use of advanced methodologies and interoperability between these domains of hospitals will aid in reducing the number of fraudulent claims, further boosting the market growth.
Restraints/Challenges
- Threat of cyber crimes
Concerns over the privacy of the patient's medical history and other personal information have grown as a result of the rise in cybercrime over the past few years. The Indiana Attorney General reported in 2015 that a cyberattack on the Indiana-based company Medical Informatics Engineering compromised the data of more than four million patients from 230 institutions (MIE). Malware, phishing, Man in the Middle attacks, Trojans, and other rising cyber threats are among those limiting market expansion to some extent.
This healthcare claims management market report provides details of new recent developments, trade regulations, import-export analysis, production analysis, value chain optimization, market share, impact of domestic and localized market players, analyses opportunities in terms of emerging revenue pockets, changes in market regulations, strategic market growth analysis, market size, category market growths, application niches and dominance, product approvals, product launches, geographic expansions, technological innovations in the market. To gain more info on the healthcare claims management market contact Data Bridge Market Research for an Analyst Brief, our team will help you take an informed market decision to achieve market growth.
COVID-19 Impact on the Healthcare Claims Management Market
The pandemic of COVID-19 is expected to have a significant impact on market growth. Since the beginning of the pandemic, there has been tremendous pressure on claim management software developers and providers due to the large number of people becoming infected and then being admitted to hospitals. Claim denials have also increased as a result of the COVID-19 pandemic. COVID-19 had a positive impact on the market. During the COVID-19 pandemic, the general impairment of health for those with SARS-CoV-2 infection lead to increase in claim management solutions, as physiological impact of the pandemic increases the claims related to the healthcare.
Recent developments
- In February 2022, Health Edge and Citius Tech formed a strategic partnership to provide joint go-to-market implementation and consultation services for HealthEdge solutions in Core administration, care management, and payment integrity to health plans pursuing value-based care and streamlined operations.
- In December 2021, HealthEdge Software completed its previously announced acquisition of well frame Inc, a leading digital health management platform.
Global Healthcare Claims Management Market Scope
The healthcare claims management market is segmented on the basis of type, component, delivery mode and end user. The growth amongst these segments will help you analyze meagre growth segments in the industries and provide the users with a valuable market overview and market insights to help them make strategic decisions for identifying core market applications.
Type
- Integrated Solutions
- Standalone Solutions
Component
- Services
- Software
Delivery Mode
- On-Premise Delivery Mode
- Cloud-Based Delivery Mode
End User
- Healthcare Payers
- Healthcare Providers
- Others
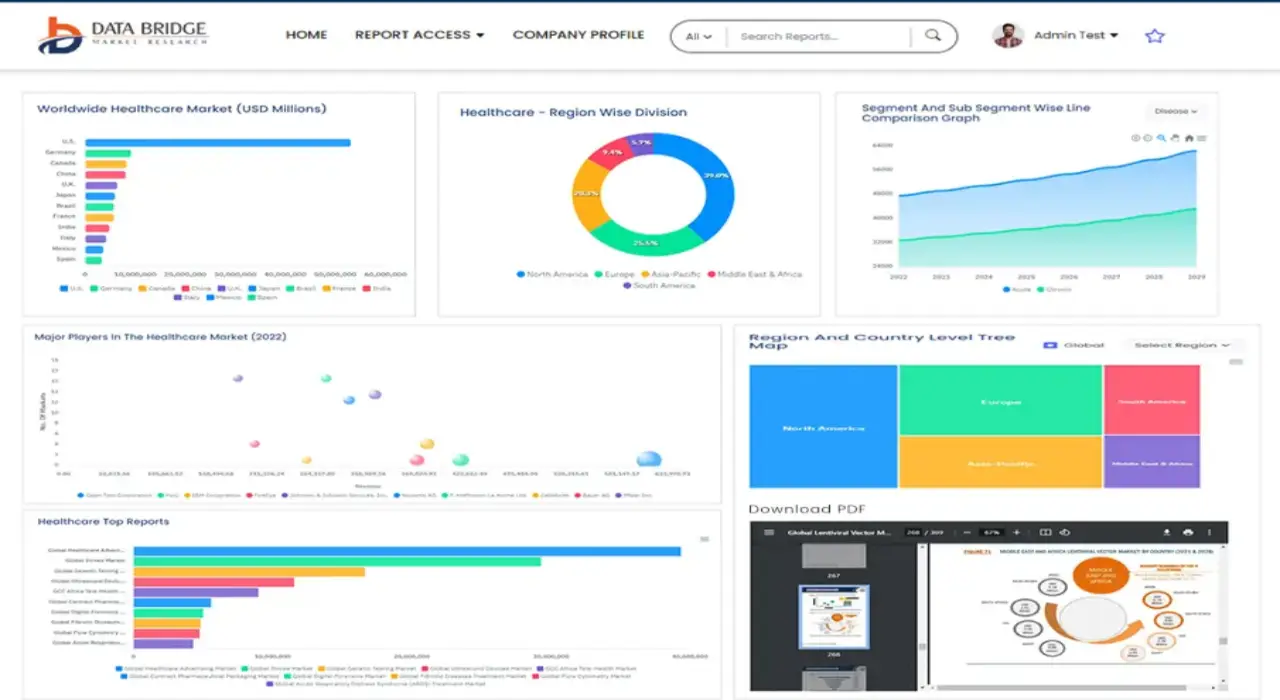
Healthcare Claims Management Market Regional Analysis/Insights
The healthcare claims management market is analyzed and market size insights and trends are provided by country, type, component, delivery mode and end user as referenced above.
The countries covered in the healthcare claims management market report are U.S., Canada and Mexico in North America, Germany, France, U.K., Netherlands, Switzerland, Belgium, Russia, Italy, Spain, Turkey, Rest of Europe in Europe, China, Japan, India, South Korea, Singapore, Malaysia, Australia, Thailand, Indonesia, Philippines, Rest of Asia-Pacific (APAC) in the Asia-Pacific (APAC), Saudi Arabia, U.A.E, South Africa, Egypt, Israel, Rest of Middle East and Africa (MEA) as a part of Middle East and Africa (MEA), Brazil, Argentina and Rest of South America as part of South America.
North America dominates the healthcare claims management market because of the presence of well-developed healthcare infrastructure and favourable reimbursement policies in the region.
Asia-Pacific is expected to grow at the highest growth rate in the forecast period of 2023 to 2030 owing to the growing healthcare infrastructure.
The country section of the report also provides individual market impacting factors and changes in regulation in the market domestically that impacts the current and future trends of the market. Data points like down-stream and upstream value chain analysis, technical trends and porter's five forces analysis, case studies are some of the pointers used to forecast the market scenario for individual countries. Also, the presence and availability of global brands and their challenges faced due to large or scarce competition from local and domestic brands, impact of domestic tariffs and trade routes are considered while providing forecast analysis of the country data.
Healthcare Infrastructure Growth Installed base and New Technology Penetration
The healthcare claims management market also provides you with detailed market analysis for every country growth in healthcare expenditure for capital equipment, installed base of different kind of products for healthcare claims management market, impact of technology using life line curves and changes in healthcare regulatory scenarios and their impact on the healthcare claims management market. The data is available for historic period 2011-2021.
Competitive Landscape and Healthcare Claims Management Market Share Analysis
The healthcare claims management market competitive landscape provides details by competitor. Details included are company overview, company financials, revenue generated, market potential, investment in research and development, new market initiatives, global presence, production sites and facilities, production capacities, company strengths and weaknesses, product launch, product width and breadth, application dominance. The above data points provided are only related to the companies' focus related to healthcare claims management market.
Some of the major players operating in the healthcare claims management market are:
- Athenahealth (U.S.)
- Plexis Healthcare Systems Inc. (U.S.)
- Cognizant (U.S.)
- Oracle (U.S.)
- Allscripts Healthcare LLC (U.S.)
- nThrive Revenue Systems, LLC (U.S.)
- eClinicalWorks (U.S.)
- Context Healthcare Inc. (U.S.)
- Optum, Inc. (U.S.)
- Mckesson Corporation (U.S.)
- DST Systems (U.S.)
- Ram Technologies Inc. (U.S.)
- General Electric (U.S.)
- Health Solutions Plus (HSP) (U.S.)
- Conifer Health Solutions, LLC (U.S.)
- Quest Diagnostics Incorporated (U.S.)
- Gebbs Healthcare Solutions (India)
- The SSI Group, LLC (U.S.)
SKU-
Get online access to the report on the World's First Market Intelligence Cloud
- Interactive Data Analysis Dashboard
- Company Analysis Dashboard for high growth potential opportunities
- Research Analyst Access for customization & queries
- Competitor Analysis with Interactive dashboard
- Latest News, Updates & Trend analysis
- Harness the Power of Benchmark Analysis for Comprehensive Competitor Tracking
Table of Content
1 INTRODUCTION
1.1 OBJECTIVES OF THE STUDY
1.2 MARKET DEFINITION
1.3 OVERVIEW OF GLOBAL HEALTHCARE CLAIMS MANAGEMENT MARKET
1.4 CURRENCY AND PRICING
1.5 LIMITATION
1.6 MARKETS COVERED
2 MARKET SEGMENTATION
2.1 KEY TAKEAWAYS
2.2 ARRIVING AT THE GLOBAL HEALTHCARE CLAIMS MANAGEMENT MARKET
2.2.1 VENDOR POSITIONING GRID
2.2.2 TECHNOLOGY LIFE LINE CURVE
2.2.3 MARKET GUIDE
2.2.4 COMPANY POSITIONING GRID
2.2.5 COMAPANY MARKET SHARE ANALYSIS
2.2.6 MULTIVARIATE MODELLING
2.2.7 TOP TO BOTTOM ANALYSIS
2.2.8 STANDARDS OF MEASUREMENT
2.2.9 VENDOR SHARE ANALYSIS
2.2.10 DATA POINTS FROM KEY PRIMARY INTERVIEWS
2.2.11 DATA POINTS FROM KEY SECONDARY DATABASES
2.3 GLOBAL HEALTHCARE CLAIMS MANAGEMENT MARKET: RESEARCH SNAPSHOT
2.4 ASSUMPTIONS
3 MARKET OVERVIEW
3.1 DRIVERS
3.2 RESTRAINTS
3.3 OPPORTUNITIES
3.4 CHALLENGES
4 EXECUTIVE SUMMARY
5 PREMIUM INSIGHT
5.1 PORTERS FIVE FORCES
5.2 REGULATORY STANDARDS
5.3 TECHNOLOGICAL TRENDS
5.4 CASE STUDY
5.5 VALUE CHAIN ANALYSIS
5.6 COMPANY COMPARITIVE ANALYSIS
6 GLOBAL HEALTHCARE CLAIMS MANAGEMENT MARKET, BY OFFERING
6.1 OVERVIEW
6.2 SOFTWARE
6.2.1 INTEGRATED
6.2.2 STAND ALONE
6.3 SERVICES
6.3.1 MANAGED SERVICES
6.3.2 PROFESSIONAL SERVICES
7 GLOBAL HEALTHCARE CLAIMS MANAGEMENT MARKET, BY DEPLOYMENT MODE
7.1 OVERVIEW
7.2 CLOUD BASED
7.3 ON-PREMISE
8 GLOBAL HEALTHCARE CLAIMS MANAGEMENT MARKET, BY APPLICATION
8.1 OVERVIEW
8.2 MEDICAL BILLING
8.3 CLAIM PROCESSING
8.4 REVENUE CYCLE MANAGEMENT
8.5 REPORTING & SCHEDULING
8.6 PAYMENT TRACKING
8.7 OTHERS
9 GLOBAL HEALTHCARE CLAIMS MANAGEMENT MARKET, BY END USER
9.1 OVERVIEW
9.2 HEALTHCARE PROVIDE
9.2.1 HOSPITAL
9.2.2 AMBULATORY CARE CENTER
9.2.3 PHARMACIES
9.2.4 SURGICAL CENTER
9.2.5 OTHERS
9.3 HEALTH CARE PAYER
9.3.1 PRIVATE PAYER
9.3.2 PUBLIC PAYER
9.3.3 OTHERS
9.4 INSURANCE & FINANCIAL INSTITUTION
9.5 OTHERS
10 GLOBAL HEALTHCARE CLAIMS MANAGEMENT MARKET, BY GEOGRAPHY
10.1 GLOBAL HEALTHCARE CLAIMS MANAGEMENT MARKET, (ALL SEGMENTATION PROVIDED ABOVE IS REPRESENTED IN THIS CHAPTER BY COUNTRY)
10.1.1 NORTH AMERICA
10.1.1.1. U.S.
10.1.1.2. CANADA
10.1.1.3. MEXICO
10.1.2 EUROPE
10.1.2.1. GERMANY
10.1.2.2. FRANCE
10.1.2.3. U.K.
10.1.2.4. ITALY
10.1.2.5. SPAIN
10.1.2.6. RUSSIA
10.1.2.7. TURKEY
10.1.2.8. BELGIUM
10.1.2.9. NETHERLANDS
10.1.2.10. NORWAY
10.1.2.11. FINLAND
10.1.2.12. SWITZERLAND
10.1.2.13. DENMARK
10.1.2.14. SWEDEN
10.1.2.15. POLAND
10.1.2.16. REST OF EUROPE
10.1.3 ASIA PACIFIC
10.1.3.1. JAPAN
10.1.3.2. CHINA
10.1.3.3. SOUTH KOREA
10.1.3.4. INDIA
10.1.3.5. AUSTRALIA
10.1.3.6. NEW ZEALAND
10.1.3.7. SINGAPORE
10.1.3.8. THAILAND
10.1.3.9. MALAYSIA
10.1.3.10. INDONESIA
10.1.3.11. PHILIPPINES
10.1.3.12. TAIWAN
10.1.3.13. VIETNAM
10.1.3.14. REST OF ASIA PACIFIC
10.1.4 SOUTH AMERICA
10.1.4.1. BRAZIL
10.1.4.2. ARGENTINA
10.1.4.3. REST OF SOUTH AMERICA
10.1.5 MIDDLE EAST AND AFRICA
10.1.5.1. SOUTH AFRICA
10.1.5.2. EGYPT
10.1.5.3. SAUDI ARABIA
10.1.5.4. U.A.E
10.1.5.5. OMAN
10.1.5.6. BAHRAIN
10.1.5.7. ISRAEL
10.1.5.8. KUWAIT
10.1.5.9. QATAR
10.1.5.10. REST OF MIDDLE EAST AND AFRICA
10.2 KEY PRIMARY INSIGHTS: BY MAJOR COUNTRIES
11 GLOBAL HEALTHCARE CLAIMS MANAGEMENT MARKET, COMPANY LANDSCAPE
11.1 COMPANY SHARE ANALYSIS: GLOBAL
11.2 COMPANY SHARE ANALYSIS: NORTH AMERICA
11.3 COMPANY SHARE ANALYSIS: EUROPE
11.4 COMPANY SHARE ANALYSIS: ASIA PACIFIC
11.5 MERGERS & ACQUISITIONS
11.6 NEW PRODUCT DEVELOPMENT AND APPROVALS
11.7 EXPANSIONS
11.8 REGULATORY CHANGES
11.9 PARTNERSHIP AND OTHER STRATEGIC DEVELOPMENTS
12 GLOBAL HEALTHCARE CLAIMS MANAGEMENT MARKET, SWOT & DBMR ANALYSIS
13 GLOBAL HEALTHCARE CLAIMS MANAGEMENT MARKET, COMPANY PROFILE
13.1 ORACLE
13.1.1 COMPANY SNAPSHOT
13.1.2 REVENUE ANALYSIS
13.1.3 PRODUCT PORTFOLIO
13.1.4 RECENT DEVELOPMENT
13.2 ATHENAHEALTH
13.2.1 COMPANY SNAPSHOT
13.2.2 REVENUE ANALYSIS
13.2.3 PRODUCT PORTFOLIO
13.2.4 RECENT DEVELOPMENT
13.3 ADVANCEDMD, INC.
13.3.1 COMPANY SNAPSHOT
13.3.2 REVENUE ANALYSIS
13.3.3 PRODUCT PORTFOLIO
13.3.4 RECENT DEVELOPMENT
13.4 RXNT
13.4.1 COMPANY SNAPSHOT
13.4.2 REVENUE ANALYSIS
13.4.3 PRODUCT PORTFOLIO
13.4.4 RECENT DEVELOPMENT
13.5 VERADIGM LLC
13.5.1 COMPANY SNAPSHOT
13.5.2 REVENUE ANALYSIS
13.5.3 PRODUCT PORTFOLIO
13.5.4 RECENT DEVELOPMENT
13.6 ORIGAMI RISK
13.6.1 COMPANY SNAPSHOT
13.6.2 REVENUE ANALYSIS
13.6.3 PRODUCT PORTFOLIO
13.6.4 RECENT DEVELOPMENT
13.7 OPTUM, INC.
13.7.1 COMPANY SNAPSHOT
13.7.2 REVENUE ANALYSIS
13.7.3 PRODUCT PORTFOLIO
13.7.4 RECENT DEVELOPMENT
13.8 ECLAIMSTATUS
13.8.1 COMPANY SNAPSHOT
13.8.2 REVENUE ANALYSIS
13.8.3 PRODUCT PORTFOLIO
13.8.4 RECENT DEVELOPMENT
13.9 AVAILITY, LL
13.9.1 COMPANY SNAPSHOT
13.9.2 REVENUE ANALYSIS
13.9.3 PRODUCT PORTFOLIO
13.9.4 RECENT DEVELOPMENT
13.1 COGNIZANT
13.10.1 COMPANY SNAPSHOT
13.10.2 REVENUE ANALYSIS
13.10.3 PRODUCT PORTFOLIO
13.10.4 RECENT DEVELOPMENT
13.11 OSP
13.11.1 COMPANY SNAPSHOT
13.11.2 REVENUE ANALYSIS
13.11.3 PRODUCT PORTFOLIO
13.11.4 RECENT DEVELOPMENT
13.12 EXPERIAN INFORMATION SOLUTIONS, INC
13.12.1 COMPANY SNAPSHOT
13.12.2 REVENUE ANALYSIS
13.12.3 PRODUCT PORTFOLIO
13.12.4 RECENT DEVELOPMENT
13.13 SMART DATA SOLUTIONS
13.13.1 COMPANY SNAPSHOT
13.13.2 REVENUE ANALYSIS
13.13.3 PRODUCT PORTFOLIO
13.13.4 RECENT DEVELOPMENT
13.14 VASTEDGE INC
13.14.1 COMPANY SNAPSHOT
13.14.2 REVENUE ANALYSIS
13.14.3 PRODUCT PORTFOLIO
13.14.4 RECENT DEVELOPMENT
13.15 CHANGE HEALTHCARE
13.15.1 COMPANY SNAPSHOT
13.15.2 REVENUE ANALYSIS
13.15.3 PRODUCT PORTFOLIO
13.15.4 RECENT DEVELOPMENT
13.16 WAYSTAR
13.16.1 COMPANY SNAPSHOT
13.16.2 REVENUE ANALYSIS
13.16.3 PRODUCT PORTFOLIO
13.16.4 RECENT DEVELOPMENT
13.17 KAREO, INC
13.17.1 COMPANY SNAPSHOT
13.17.2 REVENUE ANALYSIS
13.17.3 PRODUCT PORTFOLIO
13.17.4 RECENT DEVELOPMENT
13.18 DRCHRONO INC
13.18.1 COMPANY SNAPSHOT
13.18.2 REVENUE ANALYSIS
13.18.3 PRODUCT PORTFOLIO
13.18.4 RECENT DEVELOPMENT
13.19 NXGN MANAGEMENT, LLC
13.19.1 COMPANY SNAPSHOT
13.19.2 REVENUE ANALYSIS
13.19.3 PRODUCT PORTFOLIO
13.19.4 RECENT DEVELOPMENT
13.2 THERAPYNOTES, LLC
13.20.1 COMPANY SNAPSHOT
13.20.2 REVENUE ANALYSIS
13.20.3 PRODUCT PORTFOLIO
13.20.4 RECENT DEVELOPMENT
13.21 ECLINICALWORKS
13.21.1 COMPANY SNAPSHOT
13.21.2 REVENUE ANALYSIS
13.21.3 PRODUCT PORTFOLIO
13.21.4 RECENT DEVELOPMENT
13.22 PLEXIS HEALTHCARE SYSTEMS
13.22.1 COMPANY SNAPSHOT
13.22.2 REVENUE ANALYSIS
13.22.3 PRODUCT PORTFOLIO
13.22.4 RECENT DEVELOPMENT
13.23 MCKESSON CORPORATION
13.23.1 COMPANY SNAPSHOT
13.23.2 REVENUE ANALYSIS
13.23.3 PRODUCT PORTFOLIO
13.23.4 RECENT DEVELOPMENT
13.24 RAM TECHNOLOGIES, INC
13.24.1 COMPANY SNAPSHOT
13.24.2 REVENUE ANALYSIS
13.24.3 PRODUCT PORTFOLIO
13.24.4 RECENT DEVELOPMENT
13.25 CONIFER HEALTH SOLUTIONS, LLC
13.25.1 COMPANY SNAPSHOT
13.25.2 REVENUE ANALYSIS
13.25.3 PRODUCT PORTFOLIO
13.25.4 RECENT DEVELOPMENT
13.26 THE SSI GROUP
13.26.1 COMPANY SNAPSHOT
13.26.2 REVENUE ANALYSIS
13.26.3 PRODUCT PORTFOLIO
13.26.4 RECENT DEVELOPMENT
13.27 QUEST DIAGNOSTICS INCORPORATED
13.27.1 COMPANY SNAPSHOT
13.27.2 REVENUE ANALYSIS
13.27.3 PRODUCT PORTFOLIO
13.27.4 RECENT DEVELOPMENT
13.28 GENTEM
13.28.1 COMPANY SNAPSHOT
13.28.2 REVENUE ANALYSIS
13.28.3 PRODUCT PORTFOLIO
13.28.4 RECENT DEVELOPMENT
13.29 ATHELAS INCORPORATED
13.29.1 COMPANY SNAPSHOT
13.29.2 REVENUE ANALYSIS
13.29.3 PRODUCT PORTFOLIO
13.29.4 RECENT DEVELOPMENT
13.3 CHANGE HEALTHCARE
13.30.1 COMPANY SNAPSHOT
13.30.2 REVENUE ANALYSIS
13.30.3 PRODUCT PORTFOLIO
13.30.4 RECENT DEVELOPMENT
13.31 EZCLAIM
13.31.1 COMPANY SNAPSHOT
13.31.2 REVENUE ANALYSIS
13.31.3 PRODUCT PORTFOLIO
13.31.4 RECENT DEVELOPMENT
NOTE: THE COMPANIES PROFILED IS NOT EXHAUSTIVE LIST AND IS AS PER OUR PREVIOUS CLIENT REQUIREMENT. WE PROFILE MORE THAN 100 COMPANIES IN OUR STUDY AND HENCE THE LIST OF COMPANIES CAN BE MODIFIED OR REPLACED ON REQUEST
14 CONCLUSION
15 QUESTIONNAIRE
16 RELATED REPORTS

Research Methodology
Data collection and base year analysis are done using data collection modules with large sample sizes. The stage includes obtaining market information or related data through various sources and strategies. It includes examining and planning all the data acquired from the past in advance. It likewise envelops the examination of information inconsistencies seen across different information sources. The market data is analysed and estimated using market statistical and coherent models. Also, market share analysis and key trend analysis are the major success factors in the market report. To know more, please request an analyst call or drop down your inquiry.
The key research methodology used by DBMR research team is data triangulation which involves data mining, analysis of the impact of data variables on the market and primary (industry expert) validation. Data models include Vendor Positioning Grid, Market Time Line Analysis, Market Overview and Guide, Company Positioning Grid, Patent Analysis, Pricing Analysis, Company Market Share Analysis, Standards of Measurement, Global versus Regional and Vendor Share Analysis. To know more about the research methodology, drop in an inquiry to speak to our industry experts.
Customization Available
Data Bridge Market Research is a leader in advanced formative research. We take pride in servicing our existing and new customers with data and analysis that match and suits their goal. The report can be customized to include price trend analysis of target brands understanding the market for additional countries (ask for the list of countries), clinical trial results data, literature review, refurbished market and product base analysis. Market analysis of target competitors can be analyzed from technology-based analysis to market portfolio strategies. We can add as many competitors that you require data about in the format and data style you are looking for. Our team of analysts can also provide you data in crude raw excel files pivot tables (Fact book) or can assist you in creating presentations from the data sets available in the report.