Pregnant women and their unborn children may be impacted by opioid use. Pregnant women may misuse prescription opioids, take them as directed, or use illegal opioids like heroin. Patients must be informed about treatment options for opioid use disorder, including medicine, as well as potential dangers associated with opioid use during pregnancy. According to the most current estimate, from 2010 to 2017, there was a 131% increase in pregnant women with illnesses associated with opioids. Self-reported data from 2019 show that 7% of pregnant women reported using prescribed opioid painkillers. One in five reported misuse (defined by this survey as getting prescription opioid pain relievers from a source other than a healthcare provider or using them for a reason other than to relieve pain).
What is Opioid Use Disorder?
Heroin, improperly used or diverted prescription opioids, or other morphine-like substances may all be a part of opioid use disorder (OUD). OUD during pregnancy carries significant dangers for the mother, the foetus, and the newborn. These dangers stem from factors connected to opioid usage as well as repeated opioid exposure (such as the risk of overdose) (such as smoking, poor nutrition, needle sharing, unstable lifestyle).
Our DBMR team investigated the opioid use disorder market and it was witnessed that North America dominates the opioid use disorder market due to the initiatives by the government and the presence of prominent players within the region. Asia-Pacific is expected to witness significant growth during the forecast period of 2021 to 2028 because of the rise in awareness in the region.
To know more about the study, kindly visit: https://www.databridgemarketresearch.com/reports/global-opioid-use-disorder-market
Pregnant patients are advised to take OUD (MOUD) medication and close, supportive clinical follow-up. Providing a path to recovery, facilitating prenatal care, and assisting patients in avoiding the numerous hazards connected with the unstable lifestyle linked with substance use are all objectives (such as drug-related criminal activity, housing instability, intimate partner violence, infectious disease). The DSM-5 lists 11 primary symptoms of opioid use disorder and bases the severity on the number of recurrent symptoms encountered over a year. Mild (two to three symptoms), moderate (four to five symptoms), and severe (six or more symptoms) are the three levels of severity. The terms for abuse and dependence do not quite correspond to the new classifications of mild, moderate, and severe opioid use disorder.
Data Statistics
Opioid use in pregnancy has escalated dramatically in recent years, paralleling the epidemic observed in the general population. Worldwide, about 275 million people (or 5.5% of the global population aged 15-64 years) used drugs at least once in 2019. Among them, about 62 million people used opioids. About 36.3 million people suffered from drug use disorders in 2019. More than 259 million opioid prescriptions were written by U.S. healthcare professionals in 2012, more than double the amount from 1998. Between 2002 and 2012, the number of people using prescription opioids improperly more than doubled, and between 2000 and 2014, the number of people dying from opioid analgesics increased by approximately 400%. Rates of heroin usage have sharply increased along with the growth in prescription opioid misuse.
Neonatal abstinence syndrome has sharply increased due to the rising prevalence of opioid use during pregnancy, going from 1.5 cases per 1,000 hospital births in 1999 to 6.0 cases per 1,000 hospital births in 2013, with an associated $1.5 billion in related annual hospital costs. In 2020, an estimated 2.7 million people aged 12 or older, in the United States had an opioid use disorder (OUD) in the past 12 months.
Ill Effects of Opioid Use on Pregnancy
Various effects of opioid use are witnessed over the years in patients. The safety of opioids during early pregnancy has been evaluated in several research studies. A relation between first-trimester use of codeine and congenital abnormalities has been found in a few studies but not in others. During pregnancy, untreated chronic addiction to heroin is related with:
- Lack of prenatal care
- Increased risk of fetal growth restriction
- Abruption placentae
- Fetal death
- Preterm labor
- Intrauterine passage of meconium.
Furthermore, this untreated addiction is also associated with engagement in high-risk activities, such as trading sex for drugs, prostitution, and criminal activities. Such behaviors lead to STIs, violence, and legal consequences such as loss of child custody, criminal proceedings, or incarceration in women.
More than 30% of pregnant women enrolled in a substance use treatment program screened positive for moderate to severe depression, and more than 40% reported symptoms of postpartum depression. In addition to this, they are at higher risk of use of other substances, which includes tobacco, and cocaine, marijuana. These women also frequently suffer from poor nutrition, and many have disrupted support systems, leading to social service needs.
Our DBMR team has investigated the postpartum depression market and witnessed that the market had a CAGR of 30.25% during the forecast period of 2022 to 2029. Also, North America dominates the postpartum depression market because of the growing presence of major key players and rising prevalence of depression among women will further propel the market's growth rate in this region. Asia-Pacific are expected to grow due to growing government initiatives and development of healthcare infrastructure in this region. Also, surging awareness about mood disorders will further propel the market's growth rate in this region.
To know more about the study, kindly visit: https://www.databridgemarketresearch.com/reports/global-postpartum-depression-market
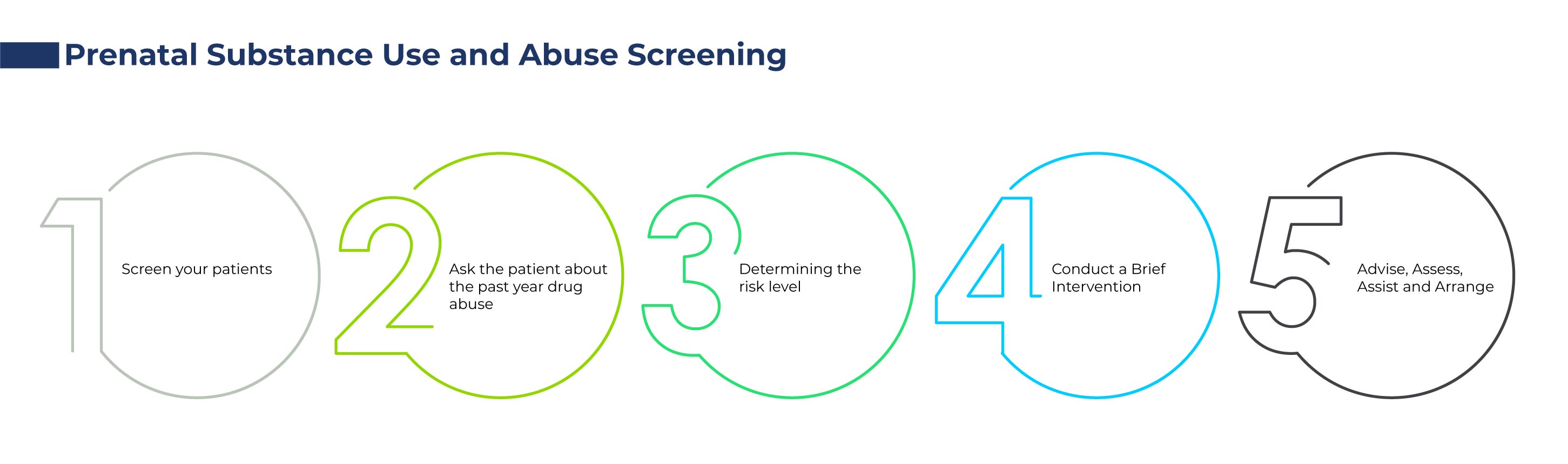
Screening for Opioid Use
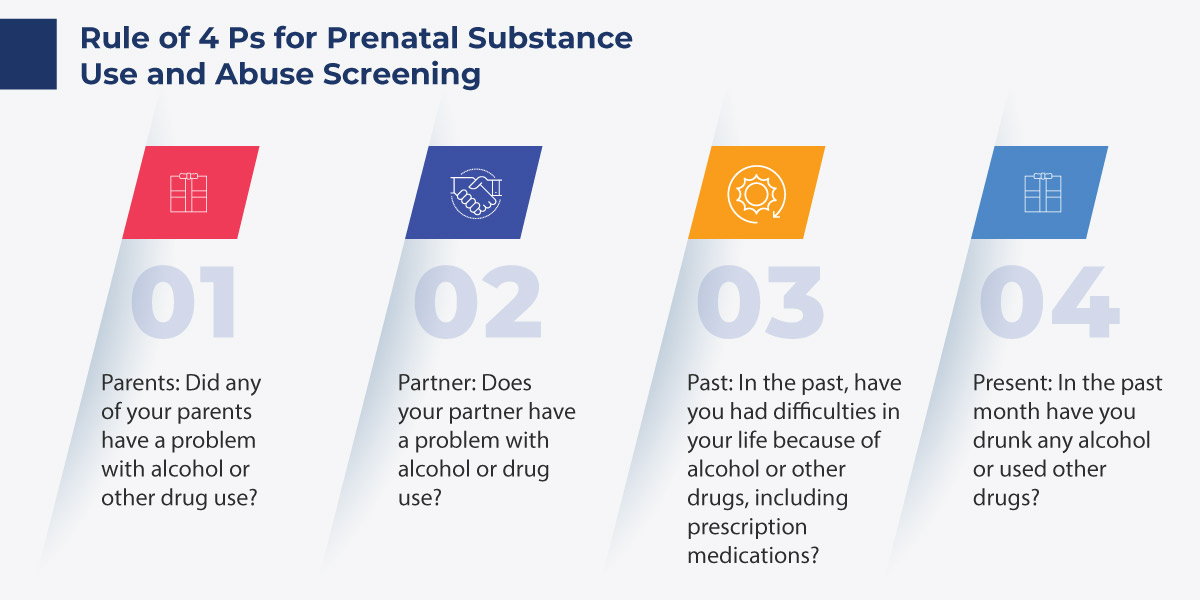
Screening should be done for all women, and they should be routinely checked. Before pregnancy and in early pregnancy, all women should be routinely asked about their usage of alcohol and drugs, which includes prescription opioids and other medications used for nonmedical reasons. Maintaining a caring and nonjudgmental approach and screening when the patient is alone are significant and will yield the most inclusive disclosure. Also, screening based only on factors such as poor adherence to prenatal care or prior adverse pregnancy outcome can lead to missed cases, and may add to stereotyping and stigma. Doctors should be well aware that reporting mandates vary widely and should be familiar with the legal requirements within their state or community.
If any of the above questions confirm an affirmative answer, then this leads to further screening and treatment processing.
Some centers have applied universal urine toxicology screening for pregnant patients, wherein one study found improved rates of detection of maternal substance use compared with standard methods. Though, this study did not use validated verbal screening tools in the comparison group, which restricts the use of these results.
What are the Possible Treatments for Opioid Use?
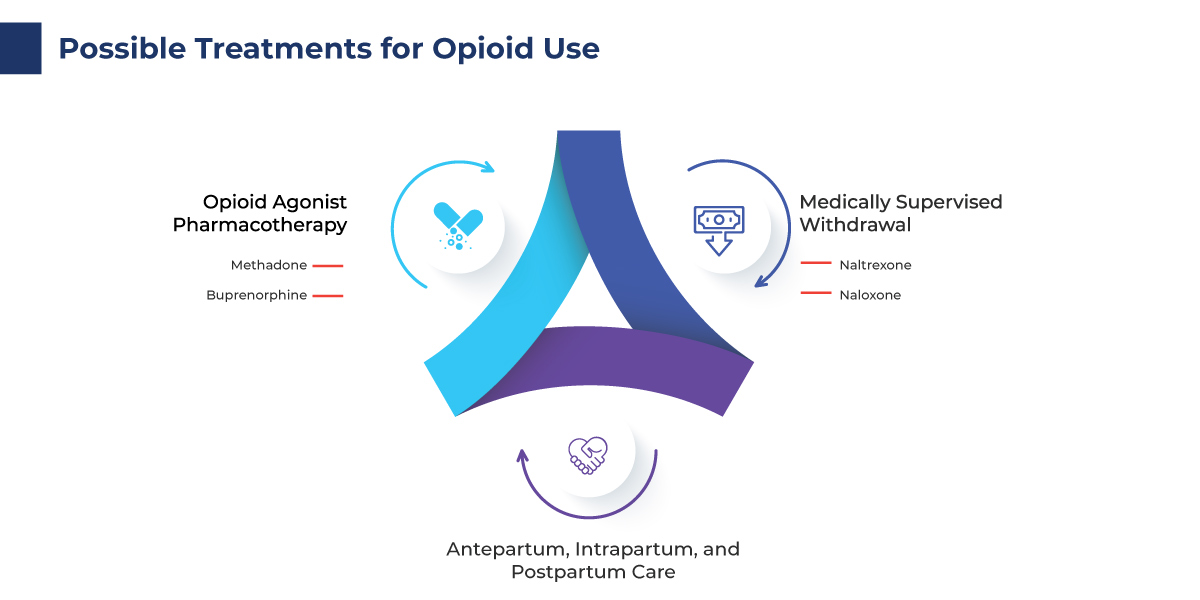
There are varied treatment options available for patients suffering from opioid use disorder during pregnancy and also after pregnancy.
There are several reasons to use opioid agonist medication while pregnant. Later, pharmacotherapy with methadone or buprenorphine was used to treat pregnant women with opioid use disorder. Additionally, it increases adherence to programs for addiction treatment and prenatal care. It has been shown that the risk of obstetric complications can be decreased by using opioid agonist pharmacotherapy along with prenatal care.
- Methadone
A daily dose of methadone is administered by an opioid treatment program that is registered, and it should be a part of comprehensive care that includes nutrition education, family therapy, addiction counseling, and other medical and psychosocial services as needed for pregnant women with opioid use disorder. To prevent withdrawal symptoms, including drug cravings, stomach cramps, nausea, insomnia, irritability, and anxiety, the methadone dosage may need to be changed throughout the pregnancy.
Case 1: If a pregnant woman starts methadone treatment, the dosage should be gradually increased until she is symptom-free in accordance with safe induction procedures. An insufficient dose of maternal methadone may cause mild to moderate opioid withdrawal symptoms and signs, which could stress the fetus and cause maternal drug cravings 43, which raise the risk of relapse and treatment termination.
Besides all these, inpatient opioid agonist therapy is started by some obstetric services using methadone or buprenorphine. Although this might make monitoring medication response more closely possible, it isn't always required or readily available. When a pregnant woman begins methadone treatment as an inpatient, a plan should be made for admission to an opioid treatment program the following day before discharge to avoid missed days. Prior to their appointment with a qualified buprenorphine prescriber, patients who started taking buprenorphine as inpatients may get a prescription. Prior to discharge, it is important to locate the ongoing buprenorphine provider and make an appointment.
- Buprenorphine
As a partial rather than a full agonist, buprenorphine works on the same mu-opioid receptors as heroin and morphine, making overdose less likely. Buprenorphine has fewer drug interactions than methadone, can be used as an outpatient treatment without requiring daily attendance at an opioid treatment program, and there is evidence that dosage adjustments aren't as frequently required during pregnancy. Furthermore, several studies show evidence of milder neonatal abstinence syndrome. To prevent any potential exposure of the fetus to naloxone during pregnancy, especially if it is administered intravenously, the buprenorphine mono-product has been advised. Recent studies that assessed the use of the combination drug of buprenorphine and naloxone, however, found no negative effects and that the results were comparable to those of buprenorphine alone.
Case 2: The pregnant woman shouldn't switch to buprenorphine if she is already receiving methadone therapy due to the high risk of accelerated withdrawal. The risk of withdrawal when switching from buprenorphine to methadone is not comparable. Any time a relatively new medication is used during pregnancy, there is a risk of unrecognized, negative long-term effects that should always be taken into account, including buprenorphine.
Medically Supervised Withdrawal
For pregnant women with an opioid use disorder, opioid agonist pharmacotherapy is the recommended therapy and is preferable to medically supervised withdrawal because withdrawal is associated with high relapse rates, ranging from 59% to more than 90%, and poorer outcomes.
Under the supervision of a doctor skilled in perinatal addiction treatment and with informed consent, medically supervised withdrawal may be considered if a woman refuses treatment with an opioid agonist or if treatment is not available. However, for this approach to be successful, a woman frequently needs prolonged inpatient care and intensive outpatient behavioral health follow-up. Opioid agonist pharmacotherapy is not widely available in some areas, so efforts should be made to make local resources more accessible. Early case reports caused concern about how opioid withdrawal during pregnancy might cause fetal stress and even death.
- Naltrexone
Naltrexone is a nonselective opioid receptor antagonist that blocks the euphoric effects of opioids and has been widely used to help nonpregnant patients with opioid use disorder to maintain abstinence. Several research on naltrexone treatment during gestation impose ethical and logistic challenges but is needed to inform the use of this treatment in pregnant patients. A latest survey among pregnant women enrolled in a comprehensive substance use treatment program shows a strong interest in considering antagonist treatment during pregnancy.
- Naloxone
Naloxone is a short-acting opioid antagonist that can rapidly reverse the effects of opioids and can be life-saving in the setting of opioid overdose. Though induced withdrawal may possibly lead to fetal stress, naloxone should be used in pregnant women in the case of maternal overdose to save the woman's life. Naloxone can be administered either intravenously or subcutaneously by health care or emergency medical professionals. Additionally, family members or other people can administer an autoinjectable form of nasal spray when overdose is suspected.
Our DBMR team investigated the nasal spray market and witnessed that the market had a CAGR of 7.10% during the forecast period 2023 to 2030. Also, North America dominates the nasal spray market due to the strong economies of the U.S. and Canada, which allow major investment in new technologies. Launching several new products, acquisitions, and partnerships, and increased incidence of chronic respiratory diseases are the primary factors boosting regional growth.
To know more about the study, kindly visit: https://www.databridgemarketresearch.com/reports/global-nasal-spray-market
Another set of care needed for these patients is a series of antepartum, intrapartum, and postpartum care.
Antepartum Care
- Consultations with anesthesia, addiction medicine specialists, pain management specialists, pediatrics,maternal–fetal medicine, behavioral health, nutrition, and social services should be conducted as needed.
- Close communication between the obstetric care provider and pediatric team before delivery is necessary for optimal management of the neonate. Neonatal consultation, if available, can be considered prenatally to discuss postdelivery care of the infant.
- Use of other substances, particularly tobacco use, is common in women with opioid use disorder. Screening for and discussion about this and other substances is important, and cessation services should be offered.
Intrapartum Care
- Women taking methadone or buprenorphine who are in labor should have their maintenance opioid agonist dose continued and should received additional pain relief.
- Some patients who are physiologically dependent on opioids may not disclose their substance use and health care providers may, thus, not be aware of their opioid use.
- Injectable nonsteroidal anti-inflammatory agents, such as ketorolac, are also very effective in pain control postpartum and postcesarean delivery.
- Regular doses of methadone or buprenorphine should be maintained during a woman's labor and postpartum hospital stay to prevent withdrawal. Patients should be advised of this plan in advance to minimize anxiety.
Postpartum Care
Breastfeeding is advantageous in women taking methadone or buprenorphine and has been related with decreased severity of neonatal abstinence syndrome symptoms, less need for pharmacotherapy, and a shorter hospital stay for the infant.
- Major dose reductions postpartum should not be done routinely but should be titrated to signs and symptoms of sedation, particularly at the peak of the dose (2–6 hours)
- Postpartum women with opioid use disorder should receive overdose training and preferably, coprescribing of naloxone for overdose prevention
- Substance use and overdose are increasingly found to be major contributing factors to pregnancy-associated deaths in the United States
Conclusion
Opioid Use Disorder are very common these days, especially in pregnant women. Early universal screening, intervention, and referral for treatment of pregnant women with opioid use and opioid use disorder improve maternal and infant outcomes. Also, contraceptive counseling and early access to contraceptive services should be a regular part of substance use disorder treatment among women of reproductive age to decrease the risk of unplanned pregnancy. Additionally, obstetric care providers have a huge responsibility to their pregnant and parenting patients suffering from substance use disorder, comforting them mentally and bringing them in good condition.